Comprehensive Guide to Cervical Cancer
In Hong Kong, many women feel anxious upon receiving gynaecological examination reports that mention terms such as "ASCUS" or "CIN," often worrying, "Does this mean I have cervical cancer?"
In fact, cervical cancer ranks seventh among the most common cancers in women in Hong Kong [Note 1]. It is a type of cancer that can be effectively detected and prevented through early screening. According to data, the cure rate for stage one cervical cancer can exceed 80% [Note 2] .
Today, we'll start with the basics of examination reports to break down cervical cancer diagnosis, treatment, and prevention methods.
Notes:
Abnormal Findings in Gynecological Examination Reports? Don't Panic—First, Learn to Interpret the Terms
Many women undergo regular check-ups without any symptoms and only discover abnormalities during these assessments. Thus, regular screenings are a crucial part of preventing cervical cancer.
Examination reports are generally divided into Pap smears (cellular examinations) and biopsy tests (tissue examinations). When you receive your report after the examination, you may encounter the following terms:
A: Pap Smear Results
-
ASCUS (Atypical Squamous Cells of Undetermined Significance)
- This means that atypical cells with slightly abnormal shapes were found in the smear, but their nature is unclear. It does not imply that you have cancer; sometimes mild inflammation can lead to this result. Doctors usually recommend further HPV testing or a follow-up examination after some time.
-
LSIL (Low-grade Squamous Intraepithelial Lesion)
- This indicates slight cellular damage, often related to HPV infection. Some women's cells may revert to normal on their own, but continuous monitoring is necessary. A colposcopy is recommended to obtain cervical tissue for further detailed examination.
-
HSIL (High-grade Squamous Intraepithelial Lesion)
- This indicates more severe cellular changes. Although it is still not cancer, it is likely classified as a high-risk type of "precancerous lesion," and immediate consultation with a gynaecological specialist for more in-depth examination is essential.

B. Biopsy Results
What is CIN?
After obtaining cervical tissue samples, doctors will perform biopsy tests, and the results are typically graded using CIN (Cervical Intraepithelial Neoplasia):
- CIN I (Mild Cervical Intraepithelial Neoplasia): This indicates slight cellular changes, which usually resolve on their own. Regular monitoring is sufficient. If the condition persists, treatment options may also be considered.
- CIN II & III (Moderate to Severe Cervical Intraepithelial Neoplasia): CIN II and III require prompt intervention. If not treated in a timely manner, they may develop into cervical cancer. For instance, with CIN III, the chance of progressing to cervical cancer within 10 years is approximately 12% [Note 3].
[Note 3] source: https://www.chp.gov.hk/files/pdf/grp-thr-report4-ch-20041209.pdf
From Pap Smear to Diagnosis: How Doctors Conduct Check-ups
When abnormal results are found in a Pap smear, it does not automatically mean cancer. To ensure an accurate diagnosis, doctors will arrange further specialized procedures:
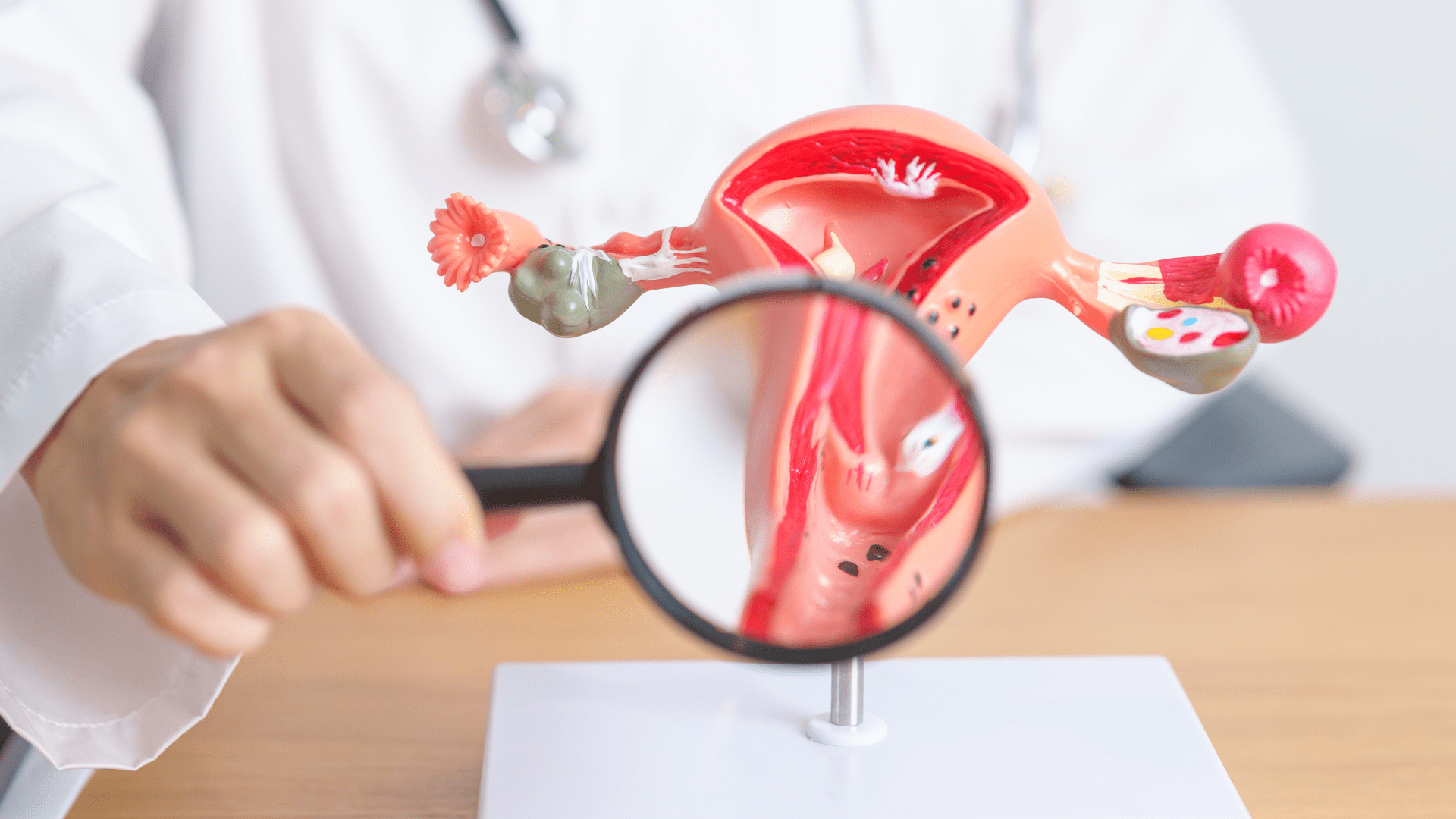
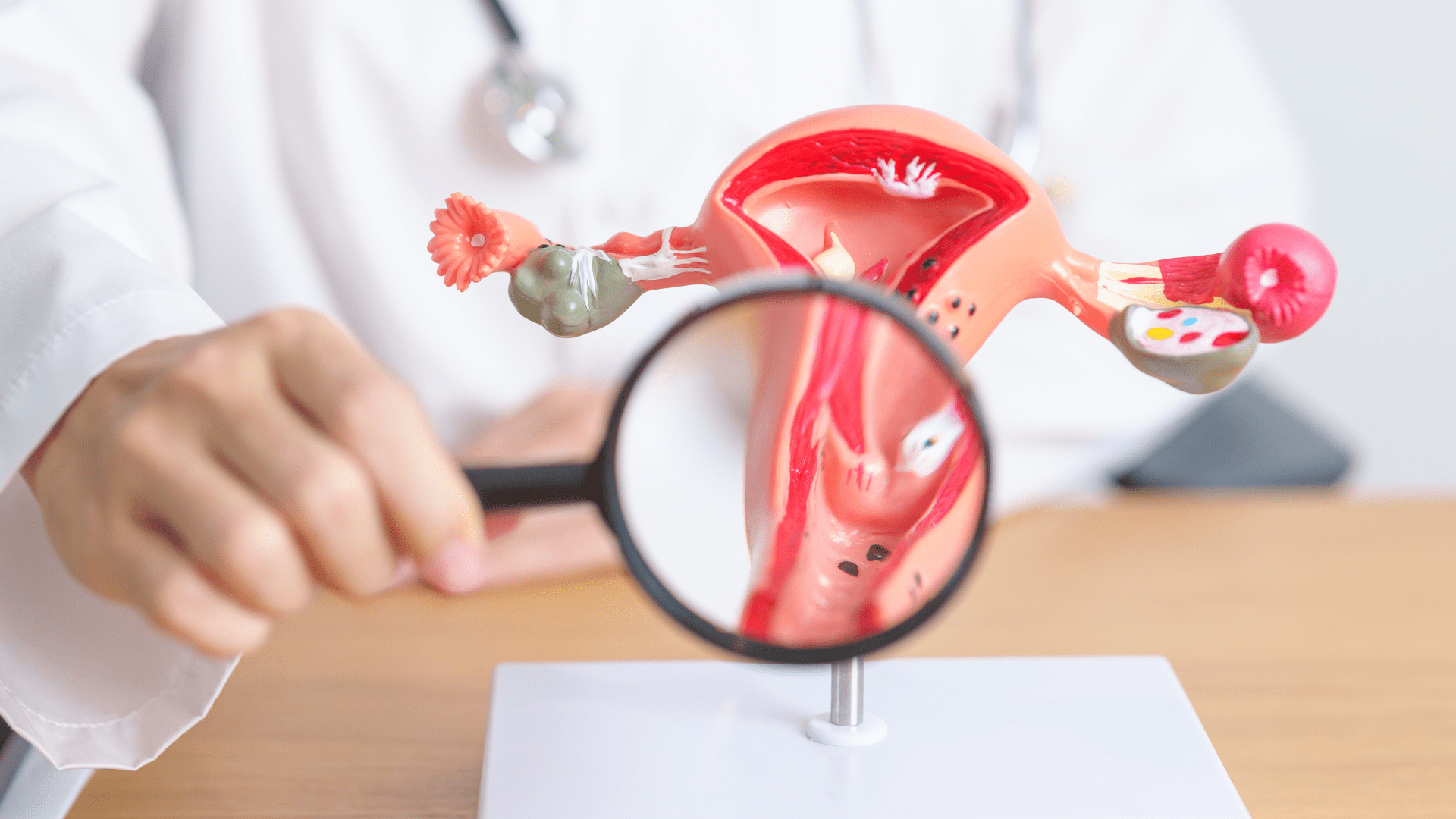
- Colposcopy: The doctor uses a microscope to magnify and examine the cervix for any abnormal lesions or visible tumors.
- Biopsy: If suspicious areas are found during the colposcopy, the doctor will take a small tissue sample to send to the laboratory for pathological examination. This is a critical step in confirming whether cancer is present.
- Imaging Tests: If cancer is confirmed, the doctor will arrange imaging studies such as MRI to determine the stage of the cancer and check for signs of metastasis.
Treatment Pathways After a Cervical Cancer Diagnosis
If cervical cancer is diagnosed, the treatment plan will depend on the cancer's stage, cell type (such as squamous cell carcinoma or adenocarcinoma), and the patient's reproductive desires.
1. Early Cervical Cancer (Surgical Treatments)
For stage one patients, surgery is the primary option:
- Conization: If the tumor is very small and the patient wishes to preserve fertility, only a portion of the cervix will be removed.
- Trachelectomy: For young women wanting to retain fertility, the cervix and surrounding tissue can be removed while keeping the main body of the uterus.
- Hysterectomy: This can be simple, modified radical, or radical. The radical hysterectomy, which involves removing the uterus, cervix, upper vagina, surrounding tissues, and pelvic lymph nodes, is the most commonly used treatment.

2. Adjuvant Therapy and Plans for Intermediate/Advanced Cancer
If post-surgery pathology reports indicate lymph node metastasis or a high risk of recurrence, adjuvant therapy will be suggested. For patients who are not suitable for surgery, the following options may also be considered:
- Radiation Therapy: Using high-energy rays to kill cancer cells.
- Chemotherapy: Usually administered alongside radiation therapy to enhance effectiveness.
- Targeted and Immunotherapy: These are applicable for more complex or advanced cases.
Frequently Asked Questions (FAQ)
-
Q1: Can I get HPV and cervical cancer if I only have one sexual partner?
A: Yes. The HPV virus is very common, and any sexual contact can lead to infection. Most people's immune systems can clear the virus, but persistent infection with high-risk HPV can lead to precancerous changes.
-
Q2: What preventive measures exist for cervical cancer?
A: Cervical cancer can be prevented through two main methods:
- - HPV Vaccination: Most cervical cancers are caused by persistent infection with high-risk human papillomavirus (HPV). Vaccination significantly reduces the risk of HPV infections.
- - Regular Screening: Cervical smears can lower the incidence of cervical cancer. Women aged 25 to 64 who have been sexually active should undergo regular screenings as advised by their doctors.
-
Q3: If I am postmenopausal and no longer sexually active, do I still need Pap smears?
A: Incorrect. The latency period for cervical cancer can be long; many cases are diagnosed in women in their 50s or 60s or after menopause. As long as there has been a history of sexual activity, regular screenings should continue, even after menopause.
-
Q4: Does an abnormal Pap smear result mean I have cancer?
A: Not necessarily. Most women with abnormal test results do not have cancer; it may be due to inflammation, atrophy, or mild precancerous cell changes. Further colposcopy and biopsy are crucial for diagnosis.
-
Q5: If a hysterectomy is needed, how long is the recovery period?
A: With current techniques, if recovery progresses smoothly, patients can typically be discharged within a few days after surgery. The doctor will schedule follow-up visits one week and one month post-surgery to assess wound healing.
Conclusion: Act Early to Protect Your Health
While cervical cancer poses a threat to women's health, its cure rate is very favourable if detected early through regular screenings. If you see abnormal data in your gynaecological report or experience unusual bleeding, consult a specialised gynaecologist promptly.
Want to learn more about the latest technologies in cervical screening or need professional interpretation of your test results?
Contact our specialist team now to schedule a consultation and examination.
Note: This article is for informational purposes only and does not constitute any medical advice. Please consult a practicing physician for any inquiries.
Updated: 2025‑01
Disclaimer: The health information on this website has been reviewed by doctors from Chiron Medical Group. The above content is for general reference only and should not be regarded as medical advice. It is not a substitute for consultation with qualified healthcare professionals about your personal health condition.